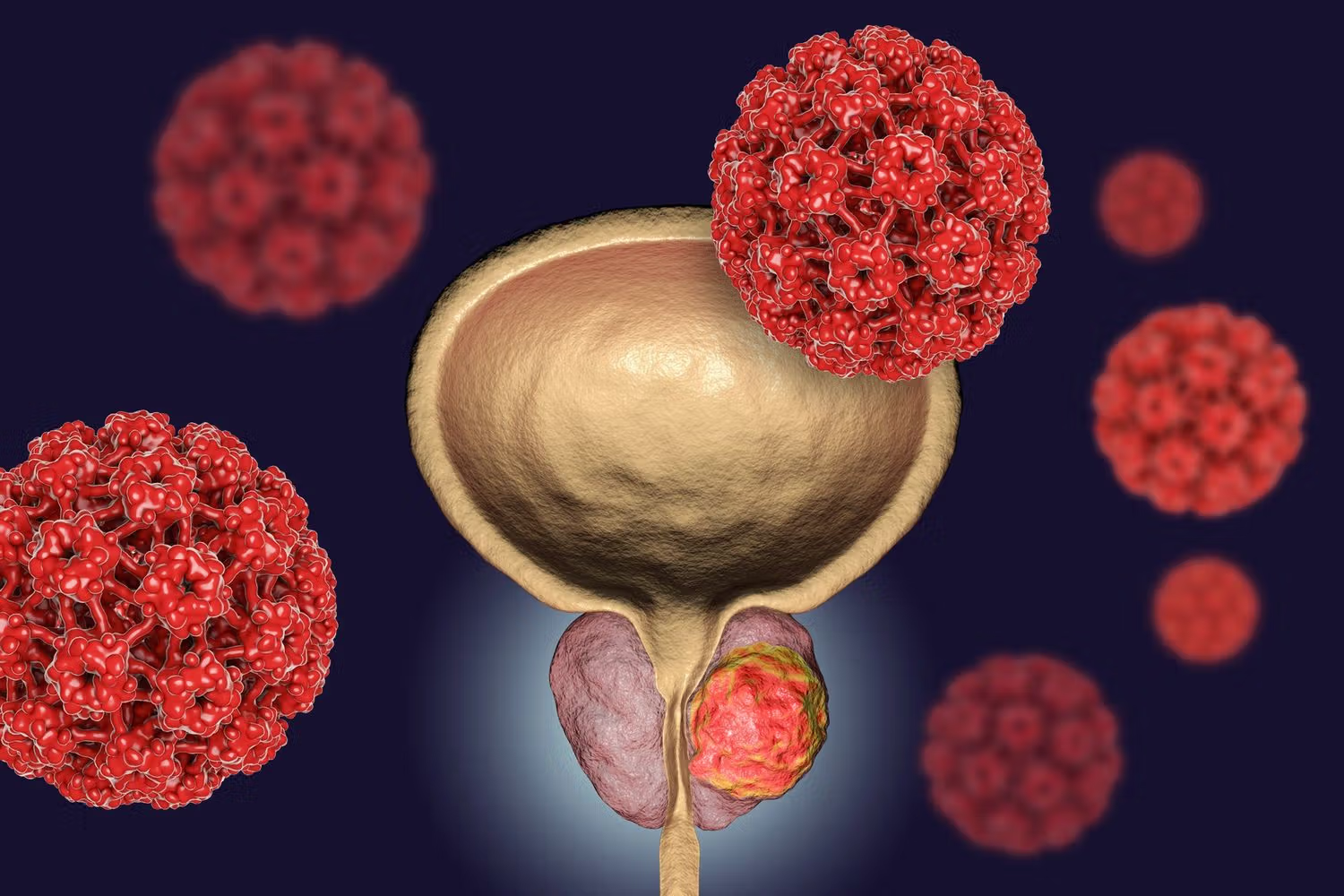
When men consider testosterone replacement therapy (TRT), concerns about prostate health often linger. Many fear that increasing testosterone could stimulate prostate growth or increase cancer risk. Yet clinical experience and advancing research suggest a more nuanced picture. In this article, we focus on TRT and prostate health—highlighting real-world insights and Debunking Myths about the risks. We offer a decidedly positive outlook, showing how a clinic in Philadelphia or elsewhere can monitor patients safely and proactively.
Understanding the Relationship: Testosterone and the Prostate
Many medical professionals once assumed that raising testosterone would unavoidably worsen prostate conditions. In truth, the relationship is complex and context-dependent. Testosterone fuels many bodily systems, and the prostate is sensitive to hormonal signaling. However, if testosterone levels are restored to mid-normal, balanced ranges (rather than pushed to supraphysiological levels), the prostate often adapts without undue stress.
Before initiating TRT, most responsible practices—including a clinic in Philadelphia experienced in men’s health—perform baseline prostate-specific antigen (PSA) testing, digital rectal exams, and imaging when indicated. Then, they vigilantly monitor PSA trends over time. In effect, they create a safety net rather than leave patients to guess.
Importantly, ongoing studies increasingly show that men with low testosterone may actually suffer more prostate “irritation” or dysregulation than men with normalized levels. In many cases, TRT allows tissues to function more stably. Indeed, by reducing inflammation and improving metabolic health, TRT may indirectly benefit prostate well-being.
As a result, numerous practices that market themselves as a clinic in Philadelphia or that advertise men’s hormone optimization stress patient education—Debunking Myths about cancer triggers, prostate enlargement, and urinary side effects. They emphasize data over fear.
Dispelling Common Fears: Debunking Myths Around TRT
Many men carry persistent misconceptions, so Debunking Myths remains a critical task. One widespread myth is that TRT invariably accelerates prostate cancer. In reality, reputable research has not demonstrated that TRT causes new prostate cancer in healthy men. Rather, individuals with undiagnosed or latent cancer might show PSA changes upon hormone normalization—but those are often detected early through proper screening.
Another myth claims that TRT causes uncontrollable prostate enlargement or worsens benign prostatic hyperplasia (BPH). Actually, most men on well-managed TRT regimens do not experience clinically significant prostate growth. In fact, by improving overall hormonal balance, TRT may reduce symptoms tied to low-tone urinary function. A clinic in Philadelphia that practices careful dose titration and follow-up can mitigate these risks.
READ THIS ALSO: Thiamine Supplement
A third myth suggests urinary symptoms always worsen after beginning TRT. On the contrary, because TRT tends to improve muscle tone, systemic inflammation, and energy levels, many men report stable or even improved urinary flow—especially when prostate health is monitored and treated as a part of overall care.
Through consistent patient education and open discussion—especially in facilities that emphasize Debunking Myths—men can pursue TRT without undue anxiety about their prostates.
How Safe Monitoring Works in Clinical Practice
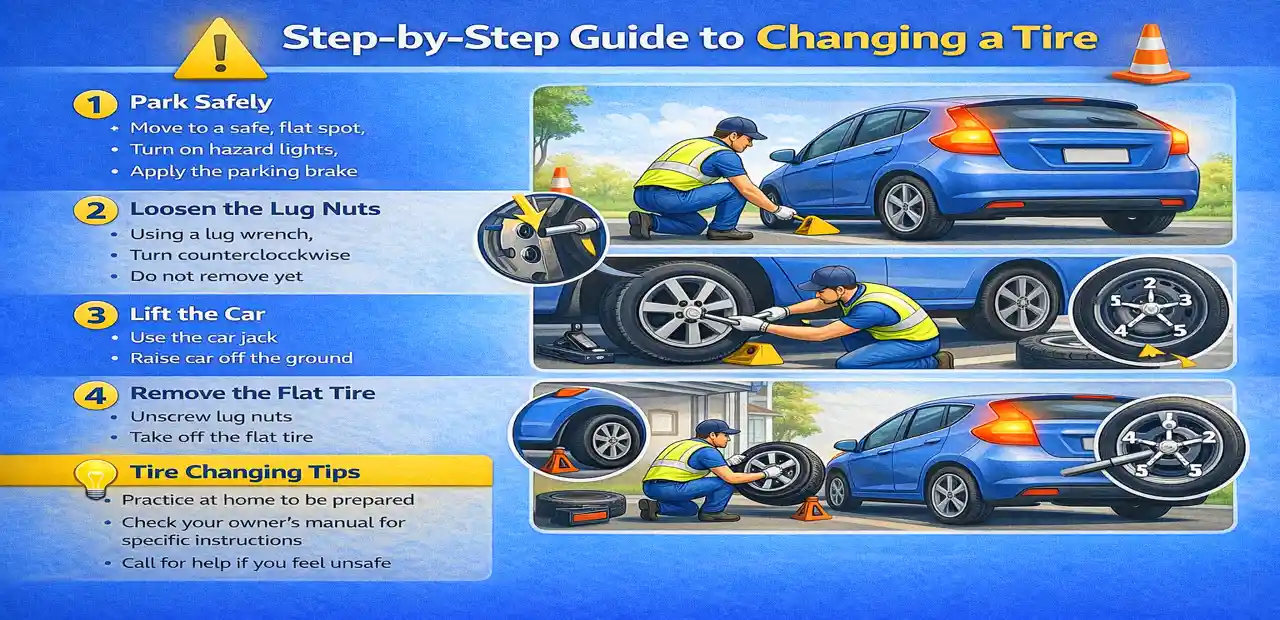
To ensure safety, clinics adopt a multi-layered monitoring approach. Initially, they gather detailed patient history—including family history of prostate disease, prior PSA values, urinary symptoms, and imaging as needed. They begin TRT only when testosterone deficiency is confirmed and no red flags exist.
Once TRT begins, patients typically undergo PSA testing every 3 to 6 months in the first year, along with periodic digital rectal exams. If any PSA rise occurs beyond expected thresholds, additional diagnostic steps follow: MRI scans or biopsy if necessary. This vigilance is often standard in a well-resourced clinic in Philadelphia or other leading centers.
Meanwhile, symptom tracking continues: urinary flow, nocturia, frequency, and any discomfort. Patients can report changes immediately, and clinicians adjust therapy accordingly. If prostate enlargement risk starts to emerge, strategies such as 5-alpha reductase inhibitors or lower testosterone dose adjustments may be employed.
Thus, the safety protocol becomes a dynamic process—not a static prescription—allowing men to benefit from TRT with minimized downside. The active approach lets clinicians address issues early rather than letting them compound unchecked.
Benefits That May Extend to the Prostate
It might seem counterintuitive, but TRT can contribute indirectly to prostate health through systemic improvements. First, optimized testosterone improves metabolic health: insulin sensitivity, fat distribution, lipid profiles, and inflammatory markers. Since metabolic syndrome and obesity often exacerbate prostate inflammation, correcting hormonal deficiency can help reduce that burden.
Second, improved muscle mass, strength, and energy facilitate better pelvic floor muscle tone and more active lifestyles. That, in turn, supports urinary tract function and may reduce lower urinary tract symptoms (LUTS) indirectly.
Third, TRT often improves mood, sleep, and vitality—factors that influence overall immune status and tissue repair. A healthier internal environment may be less permissive to abnormal growth or inflammation.
Finally, for men already under prostate care or surveillance, introducing TRT under close supervision may empower them to maintain quality of life while continuing typical prostate monitoring. In short: when responsibly administered, TRT doesn’t just preserve testosterone—it can enhance the milieu in which prostate health thrives.
Real-Life Profiles: Success Stories
Consider “Mark,” a 55-year-old man who suffered fatigue, low libido, weight gain, and mild urinary frequency. His local clinic in Philadelphia recommended baseline screening and found low testosterone levels and modestly elevated PSA. They started TRT and monitored his numbers every three months. Over the next year, his energy rebounded, urinary pattern stabilized, and PSA remained steady. He reports feeling as though a weight lifted—without any prostate complications.
Then there’s “Carlos,” age 62, who had mild BPH and borderline PSA. He wished to pursue TRT for weight and mood improvements. The clinic team explained Debunking Myths regarding prostate cancer risk. They initiated a conservative dose, watched PSA trends, and were ready to intervene if needed. After 18 months, his testosterone was back to normal, urinary symptoms improved modestly, and his PSA trajectory stayed flat.
These narratives reflect a biased but optimistic view: with care, most men achieve the hormonal balance they need without sacrificing prostate health. In fact, many see holistic benefits.
Considerations and Caveats (Yes, They Matter)
Of course, it would be irresponsible to ignore risks entirely. For men with prior prostate cancer, history of aggressive disease, or persistently rising PSA despite negative imaging, TRT may require extreme caution or avoidance. In such cases, specialized input from urologists is essential.
Additionally, overly aggressive dosing or aiming for high-end testosterone values can pose risk. That’s why a well-run practice—including a clinic in Philadelphia or elsewhere—prioritizes conservative, individualized dosing. Stability and moderation often trump extremes.
Patients must also understand that prostate issues can originate independently—aging, genetics, environmental exposures, and chronic inflammation all play roles. TRT is not a cure-all. Adopting healthy lifestyle habits, regular checkups, and early symptom reporting remain indispensable.
Ultimately, while risks exist, they are manageable when addressed proactively. This perspective underpins the optimistic tone: TRT and prostate monitoring belong in the same care plan.
A Balanced Appraisal: Why Optimism Is Justified
When one peels away sensational headlines and focuses on data and clinical experience, a more hopeful reality emerges. Debunking Myths around TRT and prostate health is not just about reassurance—it’s about aligning expectations with evidence.
Men with hypogonadism deserve treatment; they should not live with impairments due to undue fear. Moreover, as more well-monitored clinics adopt best practices, patient safety becomes normative—not fringe. A clinic in Philadelphia advertising men’s hormone balance may lead by example: offering transparency, shared decision-making, and stringent monitoring.
Yes, there will always be edge cases and uncertainties. But that’s true in every branch of medicine. With the right protocols, the benefits often outweigh the downsides. And because many patients see substantial improvements in mood, vitality, muscle mass, and overall well-being, the holistic gains can extend far beyond mere testosterone levels.
In short, viewing TRT and prostate health as adversarial is outdated. Instead, thoughtful integration—with patient education, constant vigilance, and dose flexibility—paves the way for more men to enjoy hormonal balance with peace of mind.
FAQs
Q: Does TRT cause prostate cancer?
A: No conclusive evidence proves that TRT directly causes prostate cancer in otherwise healthy men. Many perceived risks come from historical misinterpretations or outdated data. Clinics today emphasize Debunking Myths and rely on individualized risk assessment.
Q: Will TRT worsen benign prostatic hyperplasia (BPH)?
A: In many cases, appropriately dosed TRT does not precipitate worsening BPH. Some men even report stable or improved urinary function. Still, follow-up exams and symptom tracking are critical.
Q: How often should PSA be checked after starting TRT?
A: Typically, PSA is monitored every 3–6 months during the first year, then semiannually or annually depending on stability. Any concerning rise prompts further workup.
Q: Can men with a history of prostate cancer use TRT?
A: This is controversial. For men who had low-risk prostate cancer and are in long-term remission under close urological supervision, TRT may be considered cautiously. However, individuals with aggressive or recurrent disease often are excluded.
Q: Why choose a specialized clinic rather than a general office?
A: A specialized setting—such as a clinic in Philadelphia focused on men’s health—is more likely to employ rigorous monitoring, transparent patient education, and safer protocols. They are more committed to Debunking Myths and staying current with research.
Q: What lifestyle factors support prostate health while on TRT?
A: Regular exercise (particularly resistance training), healthy diet, weight management, hydration, managing metabolic syndrome, avoiding smoking, and staying current with screenings all enhance outcomes.